Avoiding tearing in delivery
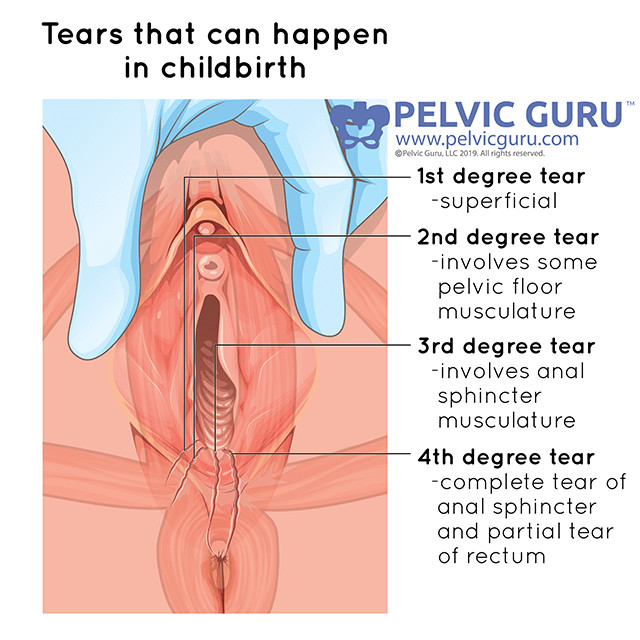
Torn pelvic floor muscles, scar. Permission to use copyright image from Pelvic Guru, LLC pelvicguru.com
These days tearing during vaginal delivery is so common it seems inevitable. It seems as thought it is a question of how far you tore, not whether or not you tore. It is possible to avoid tearing, or at least reduce the severity of the tearing, but being prepared going into delivery is important.
Complications of tearing
First, the bad news. Tearing during delivery can be associated with pain with intercourse, difficulty completing normal daily activities, urinary incontinence, and fecal incontinence. The more severe a tear is, the more likely it is to be associated with these complications. This is why it is so valuable to be prepared and to do what we can to limit severity.
Risk factors
There are a number of factors which increase the likelihood that a woman will experience a tear. Some of these factors can be avoided easily, and some are less controllable.
Woman’s position in labor:
Lying on your back or in a reclined position increases the chance of a bad tear. While it doesn’t happen often on TV, lying on your side, being up on all fours, standing, and squatting are all possible delivery positions. Being openminded and self selecting a position which is comfortable will usually help reduce the risk of a severe tear. Dr. Kate also tests every pregnant woman who she cares for to help in selecting labor position. Knowing what positions your pelvic floor relaxes best can help in selecting an easier position for the pushing phase of labor.
Baby’s position:
While this risk factor seems out of a woman’s control, you can affect your baby’s position more than may seem possible. Dr. Kate always performs ligament releases for the uterus and muscle energy techniques to the pelvis to give baby more room to move and ensure a smooth passage for baby.
Forceps delivery:
Using an instrument increases the likelihood of tearing significantly. There are cases where forceps are needed, but enabling good baby and mama position reduce the likelihood of needing forceps to deliver
Epidural:
For some, using an epidural seems unavoidable, but there are many other options for pain-relief. Epidurals limit the positions available for delivery, do not reduce sensation to the pelvic floor, and two not make it harder for baby to make its way through the birth canal. For all of these reasons, choosing to get an epidural can increase the likelihood of poor positioning, harder delivery, need for forceps, and resulting in a worse tear. These risks are important to be aware of, but it is up to every woman to make the choice whether an epidural is right for her. For some, these risks are well worth it.
Holding your breath when pushing:
It is best to push with a relaxed pelvic floor, relaxed jaw, and to breath through your pushes. Without an epidural most women will push for 5-7 seconds, 2-3 times, taking 1-2 breaths in between. If you plan to get an epidural, practice this pushing pattern with bearing down gently, but not holding your breath. Dr. Kate works on this pushing pattern with any woman planning to deliver in a hospital (based on epidural availability).
Look for a info on self scar massage, pelvic floor contractions, and healing from tears soon!
References::
Albers L, Borders N. Minimizing genital tract trauma and related birth pain following spontaneous vaginal birth. J Midwifery Womens Health. 2007; 52(3):246-253
Anderson LB, Melvaer LB, Videbech P, Lamont RF, Joergensen JS. Risk factors for developing post traumatic stress disorder following childbirth: a systematic review. Acta Obstet Gynecol Scand. 2012;91:1261-1272.
Baxley EG, Gobbo RW. Shoulder dystocia. Am Fam Physician. Apr 1, 2004;69(7):1707-14.
Beckmann MM, Garrett AJ. Antenatal perineal massage for reducing perineal trauma. Birth. 2006 Jun; 33(2):159 CochraneDatabase Syst Rev. 2006;[1]:CD005123.
Eason E, Feldman P. Preventing perineal trauma during childbirth: a systematic review. Obstet Gynecol. 2000; 95:464-71
Fitzgerald MP; Weber AM; Howden N; Cundiff GW; Brown MB. Risk factors for anal sphincter tear during vaginal delivery. Obstetrics and Gynecology. 2007 Jan; Vol. 109 (1), pp. 29-34.
Gittens-Williams L. Contemporary management of shoulder dystocia. Women’s Health. 2010;6(6):861-869.
Lieberman E, Davidson K, Lee-Parritz A, Shearer E. Changes in fetal position during labor and their association with epiduralanalgesia. Am J Obstet Gynecol. 2005; 105(5 pt 1):974-982.
Lieberman E, O’Donoghue C. Unintended effects of epidural analgesia during labor: A systematic review. Am J Obstet Gynecol.2002:186(5 Supple Nat), S31-S68.
Lowe NK. A Review of Factors Associated with Dystocia and Cesarean Section in Nulliparous Women. Journal of Midwifery &Women’s Health. 2007; 52(3):216-228.
Roberts J, The “push” for evidence: Management of the second stage. J Midwif Women’s Health. 2002:47(1);2-15.
Roberts J, Hanson L. Best practices in second stage labor care: maternal bearing down and positioning. J Midwife Women’s Health. 2007; 52(3):238-245
Schaffer J, Bloom S, Casey B, McIntire D, Nihira M, Leveno K. A randomized trial of coached bersus uncoached maternal pushing